Back surgery should be a last resort for most people who suffer back pain and sciatica. For some patients who have failed adequate conservative treatment it is a good option. But the surgery itself is only part of the treatment; just as important is the type of post surgical advice, activity, and treatment that is undertaken to ensure a full recovery.
The importance of Rehabilitation
A recent survey indicates that there are large differences among healthcare providers in the type and intensity of rehabilitation, if any, provided after lumbar surgery, as well as in the restrictions and advice given to patients in the post-operative period (McGregor, Doré, Morris, Morris, & Jamrozik, 2010).
According to a recent review on rehabilitation following lumbar decompression surgery, active post-operative programs that involve exercise lead to a faster decrease in pain and disability when compared to no treatment. There has been evidence that active treatment programs, even those involving high-intensity exercise, do not result in increased re-operation rates.
The review concluded that it is not harmful to return to activity after lumbar disc surgery, and therefore it is not necessary for patients to stay passive after their first lumbar decompression surgery (Ostelo RWJG, 2011).

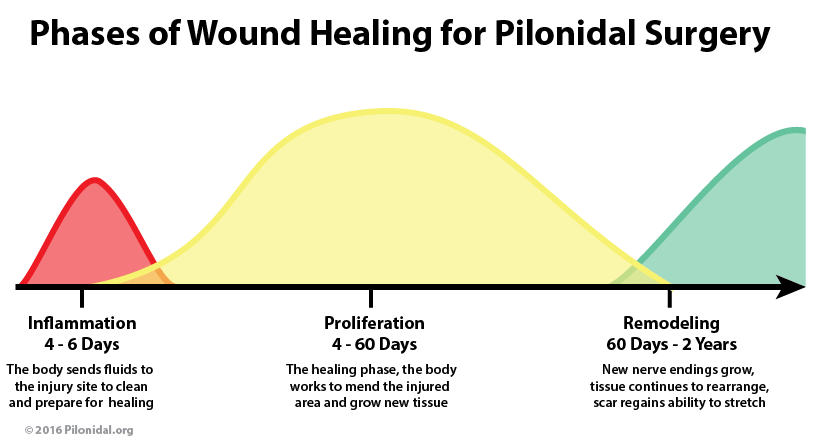
Appropriate Activity Based on Healing Phases
It is well known that early and appropriate activity enhances recovery from most surgical procedures. Especially when the surgery affects areas of the body that play a role in the way we move. The spine is no exception to this rule. The keyword is appropriate activity. The goal of a post-surgery rehab program is to keep tissues from breaking down by using early-graded activity to stop the formation of dense, inelastic scars and improve the body’s ability to handle normal activity.
Rehabilitation following lumbar decompression surgery should consist of advice and activity that is appropriate for the 3 phases of tissue healing (inflammatory, fibroplasia, and scar maturation).
Inflammatory Phase
During the initial phase of healing, advice on the avoidance of excessive stress on the healing tissues is appropriate and justified to prevent recurrent disc herniation and/or prolong the inflammatory phase of tissue healing. Within a few days, gentle, controlled movements can be initiated to enhance normal collagen formation.
The patient’s pain response and tolerance to movements and positions determine the kind and volume of controlled movement and activity. The movements typically start out gently and progress to end-range movements in loaded postures at a rate dependent on the patient’s response and stage of healing. In addition, an individualized functional restoration program to increase general strength and endurance is implemented.
Fibroplasia Phase
As long as the patient is able to tolerate them, movements can advance further during this phase.
Scar Maturation Phase
During this final phase, normal activity and movement can typically be resumed as tolerated.
Functional Outcomes
I measure the functional outcomes of the patients seen in my facility using validated health questionnaires. For postoperative lumbar spine disorders, I use the Oswestry Low Back Disability Questionnaire.
The Oswestry is scored as a percentage from 0-100, with the higher number representing a higher level of pain and disability and the lower number representing less pain and disability. A score ranging from 1-20% is considered minimally disabled, 21–40% moderately disabled, 41–60% severely disabled, 61–80% crippled, and 81–100% incapacitated. I have recorded the Oswestry sores of 99 patients treated in my facility following lumbar decompression surgeries (laminectomy, discectomy).
The average initial Oswestry score for these patients was 43% (severely disabled), and the average final Oswestry score for these patients was 20% (minimally disabled). The average number of visits to achieve these results was 14. The average duration for which these patients were seen was 7 weeks.
References
- McGregor, A., Doré, C., Morris, T., Morris, S., & Jamrozik, K. (2010). Function after spinal treatment, exercise, and rehabilitation (FASTER): improving the functional outcome of spinal surgery. BMC Musculoskeletal Disorders, 11 (17), 1–8.
- Ostelo, RWJG, C. L. (2011). Rehabilitation after lumbar disc surgery (review). The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.