Hip Pain Diagnosis Chart: Identify Causes Quickly

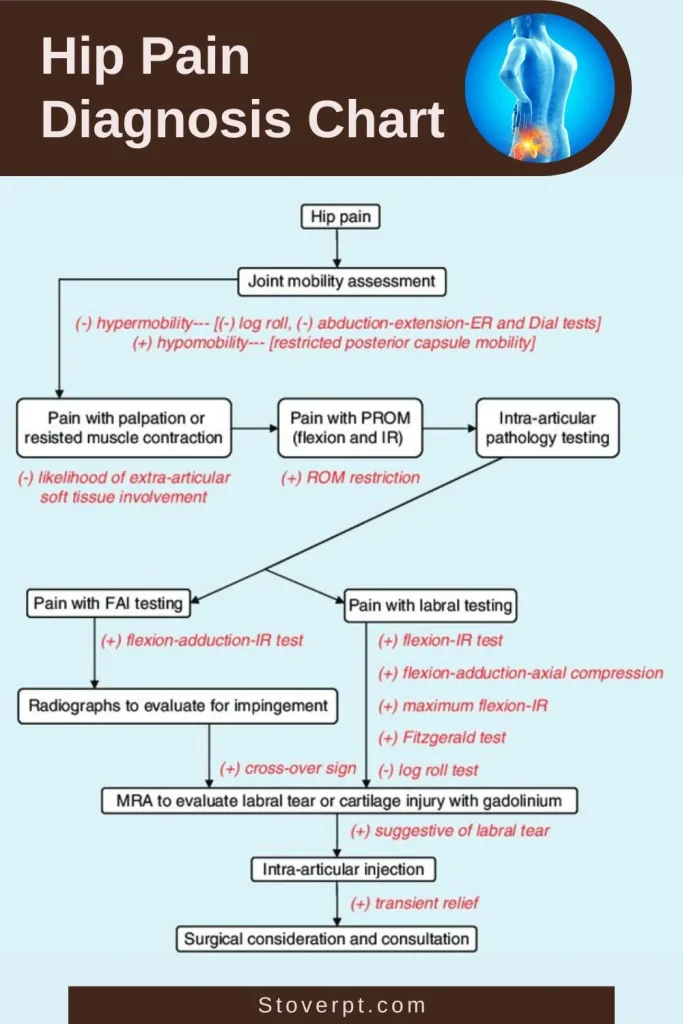
Hip pain diagnosis involves identifying the source by location, symptoms, and special tests. A diagnostic chart helps clinicians categorize pain as intra-articular (within the joint) or extra-articular (surrounding structures) to determine appropriate treatment.
Understanding Hip Pain
Hip pain is a common complaint that can significantly impact daily activities and quality of life. The hip joint is a complex structure that bears substantial weight and allows for a wide range of motion. When pain occurs in this area, it can be challenging to determine the exact cause due to the numerous structures that could be involved. A systematic approach to diagnosis is essential for effective treatment.
Anatomy of the Hip

The hip joint is a ball-and-socket joint formed by the femoral head (ball) and the acetabulum of the pelvis (socket). This design allows for significant movement in multiple planes while maintaining stability. Surrounding the joint are various structures including:
- Articular cartilage covering the femoral head and acetabulum
- Acetabular labrum, a fibrocartilaginous rim that deepens the socket
- Joint capsule and ligaments providing stability
- Muscles and tendons controlling movement
- Bursae reducing friction between moving structures
- Nerves and blood vessels supplying the region
Understanding this anatomy is crucial when diagnosing hip pain, as different structures can cause distinct pain patterns and symptoms.
Importance of Accurate Diagnosis
Accurate diagnosis of hip pain is essential for several reasons:
- It guides appropriate treatment selection
- It helps prevent unnecessary interventions
- It allows for early management of potentially serious conditions
- It provides patients with clarity about their condition
A hip pain diagnosis chart serves as a valuable tool for clinicians to systematically evaluate patients and determine the most likely cause of their symptoms.
Differential Diagnosis by Pain Location
One of the most useful approaches to diagnosing hip pain is to consider the location of the pain. Different anatomical structures typically cause pain in specific regions around the hip.
Anterior Hip Pain (Front of Hip)
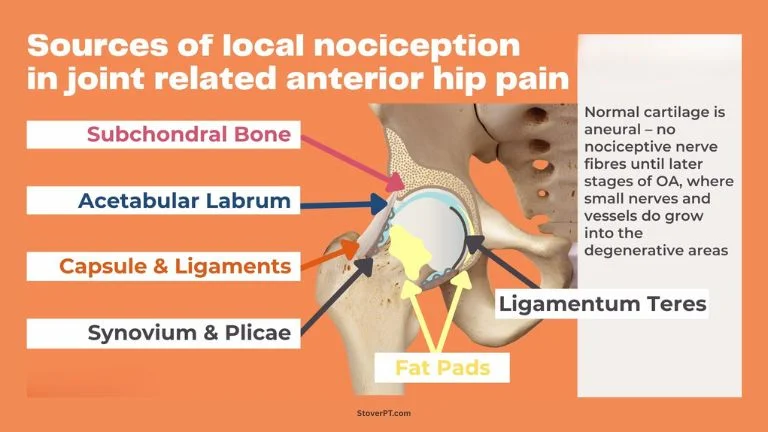
Pain in the front of the hip often indicates intra-articular pathology or issues with structures in the anterior hip region. Common causes include:
- Osteoarthritis
- Femoroacetabular impingement (FAI)
- Hip labral tears
- Iliopsoas bursitis (also known as internal snapping hip)
- Femoral neck stress fractures
- Hip flexor strains
- Osteonecrosis (avascular necrosis)
- Septic arthritis
- Transient synovitis (particularly in children)
Patients with anterior hip pain often report groin pain that may radiate to the knee. They frequently demonstrate the “C-sign” when describing their pain, cupping their hand above the greater trochanter with the thumb in the groin and fingers extending to the buttock.
Lateral Hip Pain (Side of Hip)

Pain on the side of the hip typically suggests extra-articular conditions affecting the structures around the greater trochanter. Common causes include:
- Greater trochanteric pain syndrome
- External snapping hip (iliotibial band)
- Gluteal muscle tears or avulsions
- Iliotibial band syndrome
- Trochanteric bursitis
- Hip osteoarthritis (can sometimes present with lateral pain)
Lateral hip pain is often aggravated by lying on the affected side, climbing stairs, or prolonged walking. Patients may report a snapping or clicking sensation with certain movements.
Posterior Hip Pain (Back of Hip)
Pain in the back of the hip may originate from the hip joint itself or from surrounding structures. Common causes include:
- Piriformis syndrome
- Ischiofemoral impingement
- Sacroiliac joint dysfunction
- Lumbar radiculopathy
- Hamstring muscle strains or avulsions
- Ischial bursitis
- Gluteal muscle pathology
Posterior hip pain may be confused with low back pain, and careful examination is needed to differentiate between the two.
Clinical Examination Techniques
A thorough clinical examination is essential for diagnosing the cause of hip pain. This includes a detailed history, observation, palpation, range of motion assessment, and special tests.
History Taking
The patient history provides valuable clues about the cause of hip pain. Important questions to ask include:
- When did the pain start? Was the onset sudden or gradual?
- Is there a history of trauma or injury?
- Where exactly is the pain located? Does it radiate?
- What activities aggravate or relieve the pain?
- Is there stiffness, particularly in the morning?
- Are there any clicking, catching, or locking sensations?
- Have you noticed any swelling, redness, or warmth?
- Do you have any other medical conditions?
- Are you taking any medications?
The answers to these questions can help narrow down the differential diagnosis and guide the physical examination.
Physical Examination
The physical examination for hip pain should include:
- Observation of gait, posture, and alignment
- Palpation of bony landmarks and soft tissues
- Range of motion assessment (active and passive)
- Strength testing
- Special tests specific to hip pathology
Gait Assessment
Observing the patient’s walking pattern can reveal valuable information. Look for:
- Antalgic gait (shortened stance phase on the affected side)
- Trendelenburg gait (trunk shift toward the affected side during stance phase)
- Short leg gait
- Circumduction (swinging the leg outward to avoid hip flexion)
Range of Motion Testing
Assess both active and passive range of motion in all planes:
- Flexion (normal: 120-135 degrees)
- Extension (normal: 10-30 degrees)
- Abduction (normal: 30-50 degrees)
- Adduction (normal: 10-30 degrees)
- Internal rotation (normal: 30-40 degrees)
- External rotation (normal: 40-60 degrees)
Restricted internal rotation is often one of the earliest signs of hip joint pathology, particularly in osteoarthritis.
Special Tests for Hip Pathology
Several special tests can help identify specific hip conditions:
Tests for Intra-articular Pathology
- FADIR Test (Flexion, Adduction, Internal Rotation)
- Patient supine, examiner passively flexes, adducts, and internally rotates the hip
- Positive if it reproduces the patient’s pain
- Suggests femoroacetabular impingement or labral tear
- FABER Test (Flexion, Abduction, External Rotation)
- Also known as Patrick’s test
- Patient supine, examiner places the foot of the affected leg on the opposite knee and applies gentle pressure
- Ipsilateral pain suggests hip joint pathology
- Contralateral pain suggests sacroiliac joint dysfunction
- Log Roll Test
- Patient supine, examiner rotates the extended leg internally and externally
- Positive if it causes pain
- Suggests intra-articular pathology or fracture
- Stinchfield Test
- Patient supine, examiner asks the patient to actively flex the hip against resistance
- Positive if it reproduces pain
- Suggests hip joint pathology
Tests for Extra-articular Pathology
- Ober’s Test
- Tests for iliotibial band tightness
- Patient side-lying, examiner passively abducts and extends the upper leg, then allows it to adduct
- Positive if the leg does not adduct (fall toward the table)
- Trendelenburg Test
- Patient stands on one leg
- Positive if the pelvis drops on the non-stance side
- Indicates weakness of the stance leg’s hip abductors
- Piriformis Test
- Patient supine, examiner flexes, adducts, and internally rotates the hip
- Positive if it reproduces buttock pain
- Suggests piriformis syndrome
- Compression Test
- Can be performed at the foot, knee, or lateral hip
- Examiner applies pressure along the axis of the femur
- Positive if it reproduces hip pain
- Suggests hip fracture or severe intra-articular pathology
Imaging Studies for Hip Pain
When clinical examination suggests a specific diagnosis or when further information is needed, imaging studies can be valuable. The choice of imaging modality depends on the suspected pathology.
Radiography (X-rays)
X-rays are usually the first imaging study ordered for hip pain. Standard views include:
- Anteroposterior (AP) pelvis
- AP of the affected hip
- Lateral view (frog-leg or cross-table lateral)
X-rays can detect:
- Osteoarthritis (joint space narrowing, osteophytes, subchondral sclerosis)
- Fractures
- Femoroacetabular impingement (cam or pincer lesions)
- Avascular necrosis (in later stages)
- Developmental dysplasia
- Tumors or other bony abnormalities
Magnetic Resonance Imaging (MRI)
MRI provides detailed images of soft tissues and is particularly useful for:
- Labral tears
- Cartilage damage
- Muscle or tendon injuries
- Early avascular necrosis
- Bone marrow edema
- Soft tissue masses
MR arthrography (MRI with intra-articular contrast) improves visualization of the labrum and cartilage and is often the preferred study for suspected labral tears.
Computed Tomography (CT)
CT scans provide detailed images of bony structures and are useful for:
- Complex fractures
- Bony anatomy in femoroacetabular impingement
- Preoperative planning
- Patients who cannot undergo MRI
Three-dimensional CT reconstructions can be particularly helpful in understanding complex bony abnormalities.
Ultrasound
Ultrasound is useful for evaluating superficial soft tissue structures such as:
- Bursae
- Tendons
- Joint effusions
- Guiding injections
It has the advantages of being dynamic (can assess structures during movement) and does not involve radiation.

Common Hip Pathologies and Their Diagnostic Features
Osteoarthritis
Osteoarthritis (OA) is one of the most common causes of hip pain, particularly in older adults.
Diagnostic features:
- Gradual onset of pain, typically worse with activity and improved with rest
- Morning stiffness lasting less than an hour
- Reduced internal rotation and flexion
- Pain with weight-bearing
- Radiographic findings: joint space narrowing, osteophytes, subchondral sclerosis, subchondral cysts
Femoroacetabular Impingement
Femoroacetabular impingement (FAI) occurs when there is abnormal contact between the femoral head/neck and the acetabular rim.
Types:
- Cam impingement: Abnormal femoral head-neck junction
- Pincer impingement: Overcoverage of the acetabulum
- Mixed: Combination of both
Diagnostic features:
- Typically affects young and middle-aged active individuals
- Groin pain, often with activity
- Positive impingement tests (FADIR)
- Restricted internal rotation
- Radiographic findings: cam deformity (pistol grip deformity), pincer deformity (acetabular overcoverage, crossover sign)
Labral Tears
The acetabular labrum is a fibrocartilaginous rim that deepens the hip socket and provides stability.
Diagnostic features:
- Often associated with FAI
- Deep groin pain
- Clicking, catching, or locking sensations
- Pain with pivoting activities
- Positive impingement tests
- Best visualized on MR arthrography
Avascular Necrosis
Avascular necrosis (AVN) or osteonecrosis occurs when blood supply to the femoral head is compromised, leading to bone death.
Risk factors:
- Corticosteroid use
- Alcohol abuse
- Trauma
- Sickle cell disease
- HIV infection
- Systemic lupus erythematosus
Diagnostic features:
- Sudden or gradual onset of pain
- Pain with weight-bearing
- Limited range of motion
- Early stages may have normal X-rays
- MRI shows characteristic changes even in early stages
- Later stages show femoral head collapse on X-ray (crescent sign)
Greater Trochanteric Pain Syndrome
Greater trochanteric pain syndrome (GTPS) encompasses several conditions including trochanteric bursitis, gluteal tendinopathy, and external snapping hip.
Diagnostic features:
- Lateral hip pain
- Pain with lying on the affected side
- Tenderness over the greater trochanter
- Pain with resisted hip abduction
- Positive Ober’s test may be present
- Normal X-rays
- Ultrasound or MRI may show bursal fluid or tendon abnormalities
Piriformis Syndrome
Piriformis syndrome occurs when the piriformis muscle irritates or compresses the sciatic nerve.
Diagnostic features:
- Buttock pain that may radiate down the posterior thigh
- Pain with sitting or activities that involve hip external rotation
- Tenderness in the sciatic notch
- Positive piriformis test
- Normal imaging studies (diagnosis of exclusion)
Inflammatory Arthritis
Inflammatory arthritis, such as rheumatoid arthritis, can affect the hip joint.
Diagnostic features:
- Morning stiffness lasting more than an hour
- Systemic symptoms (fatigue, fever)
- Multiple joint involvement
- Radiographic findings: concentric joint space narrowing, periarticular osteopenia, erosions
- Elevated inflammatory markers (ESR, CRP)
Septic Arthritis
Septic arthritis is a medical emergency requiring prompt diagnosis and treatment.
Diagnostic features:
- Sudden onset of severe hip pain
- Fever
- Inability to bear weight
- Marked limitation of all movements
- Joint effusion
- Elevated white blood cell count, ESR, CRP
- Diagnosis confirmed by joint aspiration
Diagnostic Algorithms for Hip Pain
A systematic approach to diagnosing hip pain can help clinicians arrive at the correct diagnosis efficiently. The following algorithm provides a framework for evaluating patients with hip pain:
- History and Physical Examination
- Determine pain location (anterior, lateral, posterior)
- Assess onset, duration, and aggravating/relieving factors
- Perform gait assessment
- Evaluate range of motion
- Conduct special tests based on suspected pathology
- Initial Imaging
- Standard radiographs (AP pelvis, AP and lateral hip)
- If fracture is suspected in the setting of normal X-rays, consider MRI
- Further Evaluation Based on Initial Findings
- If intra-articular pathology is suspected:
- Consider MRI or MR arthrography
- Consider diagnostic injection
- If extra-articular pathology is suspected:
- Consider ultrasound or MRI based on the specific structure involved
- If inflammatory condition is suspected:
- Order laboratory tests (ESR, CRP, rheumatoid factor, etc.)
- If infection is suspected:
- Urgent joint aspiration
- Blood cultures
- Laboratory tests (WBC, ESR, CRP)
- Diagnostic Injection
- Intra-articular injection of local anesthetic can help confirm if pain is originating from the hip joint
- Significant relief suggests intra-articular pathology
- Minimal or no relief suggests extra-articular source
Case Studies
Case Study 1: Femoroacetabular Impingement in a Young Athlete
A 17-year-old female basketball player presented with right lower back and groin pain after falling on her right hip during a game. She reported burning pain in the right anterior-superior thigh and occasional catching/clicking in her right hip/buttock region. Physical examination revealed limited internal rotation of the right hip (15° compared to 30° on the left) and positive tests for femoroacetabular impingement and labral tear.
Imaging studies including radiography, MRI arthrogram, and 3D CT suggested pincer impingement with cam lesion and a tear of the superior labrum. An intra-articular injection provided complete but temporary relief of symptoms, confirming intra-articular pathology.
Surgical intervention revealed intact acetabular labrum without pathologic pincer impingement but showed grade III chondromalacia of the anterolateral acetabulum with cam-type impingement. Treatment included chondroplasty of the anterior acetabulum, synovectomy of the acetabular fossa, and femoroplasty for cam impingement.
Following a structured rehabilitation program, the patient returned to competitive basketball approximately 4 months after surgery and continued without complaints 20 months post-surgery.
Case Study 2: Avascular Necrosis vs. Osteoarthritis
A 59-year-old male with a complicated medical history was referred with a diagnosis of severe bilateral hip osteoarthritis. He presented with insidious onset, severe bilateral groin and anterior thigh pain with rapid progression of functional decline.
While typical osteoarthritis has a similar presentation, patients with OA typically report a more gradual onset of symptoms with less rapid progression of disability. The patient’s clinical presentation, including the rapid progression of symptoms and multiple risk factors (HIV, corticosteroid intake), led to a differential diagnosis of bilateral avascular necrosis of the femoral heads.
Despite initial conservative management with manual physical therapy, the patient’s condition continued to deteriorate, with his Lower Extremity Functional Scale score worsening from 33 to 21 over one month. This persistence of painful symptoms and continued functional decline led to referral back to his GP for further diagnostic testing and eventual correct diagnosis.
Frequently Asked Questions
What is the most common cause of hip pain?
Osteoarthritis is the most common cause of hip pain, particularly in adults over 50 years of age. Other common causes include greater trochanteric pain syndrome, femoroacetabular impingement, and labral tears.
How can I tell if my hip pain is serious?
Signs that hip pain may be serious and require immediate medical attention include:
- Inability to bear weight on the affected leg
- Severe pain that prevents movement of the hip
- Significant swelling or bruising around the hip
- Hip pain accompanied by fever
- Hip pain following a fall or significant trauma
- Sudden onset of severe pain
Can hip pain be referred from other areas?
Yes, hip pain can be referred from other areas, particularly the lumbar spine and sacroiliac joints. Similarly, hip joint problems can sometimes present as knee pain. This is why a thorough examination of the entire kinetic chain is important in diagnosing the source of pain.
What tests are used to diagnose hip pain?
Diagnostic tests for hip pain may include:
- Physical examination and special tests (FADIR, FABER, etc.)
- X-rays to evaluate bone structure and joint spaces
- MRI or MR arthrography to assess soft tissues, cartilage, and labrum
- CT scans for detailed bone imaging
- Ultrasound for soft tissue evaluation
- Diagnostic injections to confirm the pain source
- Blood tests to check for inflammatory or infectious causes
How is hip pain treated?
Treatment depends on the specific diagnosis but may include:
- Rest and activity modification
- Physical therapy to improve strength, flexibility, and movement patterns
- Medications such as NSAIDs for pain and inflammation
- Injections (corticosteroid, hyaluronic acid, platelet-rich plasma)
- Assistive devices (cane, walker)
- Surgical interventions for certain conditions (arthroscopy, hip replacement)





