Physical Therapist vs. Physiotherapist: The Difference?

Have you ever wondered what the difference is between a physical therapist and a physiotherapist? Though the terms are sometimes used interchangeably, there are some key differences between these two careers in rehabilitative healthcare.
In this comprehensive blog post, we’ll compare physical therapists and physiotherapists in depth so you can understand the similarities and differences.
Defining Each Role
First, let’s clearly define what exactly a physical therapist and physiotherapist are:
Physical Therapist
A physical therapist (PT) is a healthcare professional who works to help patients regain mobility and reduce pain and disabilities from injuries, chronic conditions, or surgeries. They examine patients to develop treatment plans using techniques like stretching, hot and cold therapies, electrical stimulation, aquatic therapy, hands-on joint mobilization, and assisting with exercise routines.
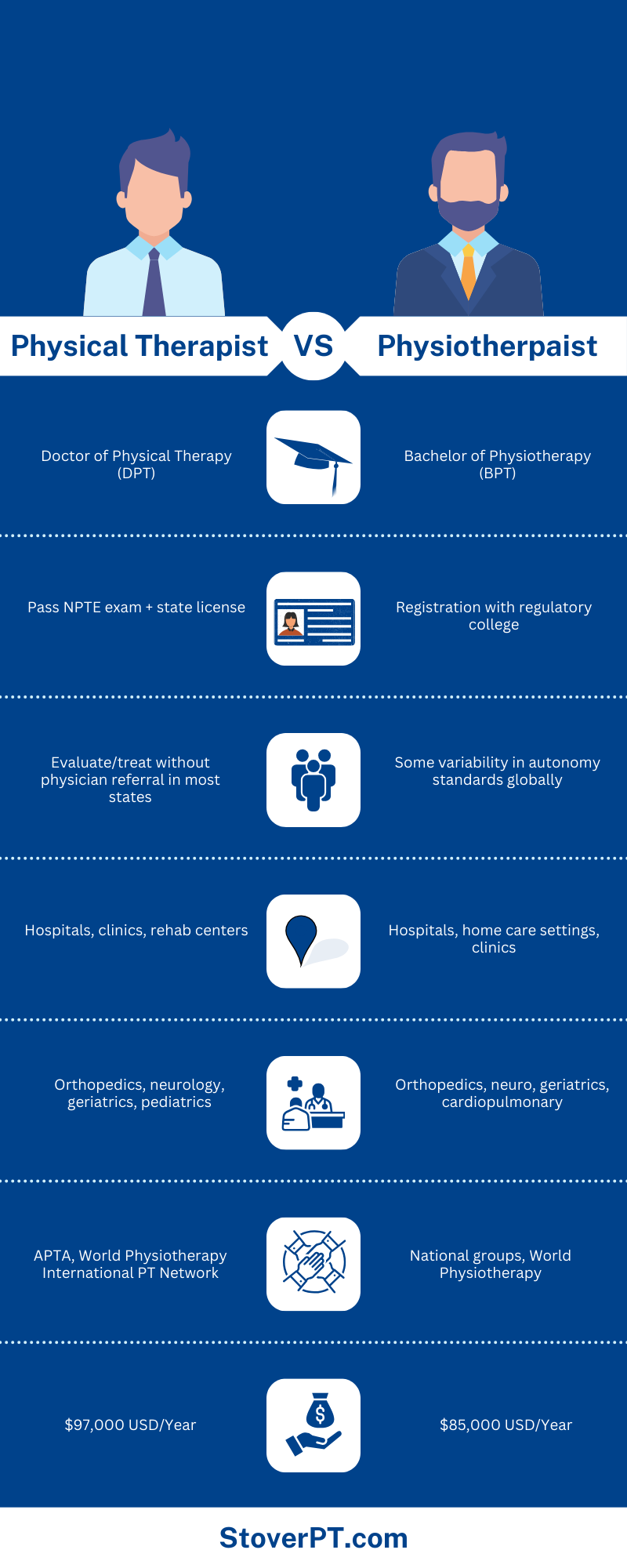
Physical therapists typically earn a Doctor of Physical Therapy (DPT) degree in the United States, which includes clinical rotations. All states require PTs to be licensed with regular renewal. There are several PT specialties like orthopedics, geriatrics, neurology, pediatrics, sports, and more that require additional certifications.
Physiotherapist
A physiotherapist has an extremely similar role to a physical therapist, assisting patients with movement dysfunctions due to illness, injury, aging, or environmental factors. However, physiotherapists complete more generalized training on the full body.
Physiotherapists typically earn a bachelor’s degree in physiotherapy with clinical work. Like PTs, physiotherapists must register with regulatory boards in most countries to demonstrate qualifications and licensure to practice. They can also complete certifications in specialty areas like sports physiotherapy, gynecology, respiratory care, and more, depending on their interests and career goals.
Education and Training: Physiotherapist vs physical therapist
As noted above, the typical education for a physical therapist vs. physiotherapist differs slightly:
Physical Therapist Education
In the United States, physical therapists typically earn a Doctor of Physical Therapy (DPT) degree, which includes clinical rotations and coursework in areas like:
- Anatomy
- Physiology
- Neuroscience
- Biomechanics
- Pathophysiology
- Patient assessment
- Treatment interventions
- Exercise prescription
A DPT program usually takes 3 years to complete after finishing a Bachelor’s degree. All states require PTs to pass the National Physical Therapy Exam (NPTE) and obtain a state license to legally practice. PTs must complete continuing education to keep licenses current.
Physiotherapist Education
In many countries, physiotherapists earn an undergraduate Bachelor’s degree specifically in Physiotherapy, which has coursework in areas like:
- Anatomy
- Physiology
- Pathology
- Biomechanics
- Electrotherapy
- Rehabilitation
- Clinical Science
In addition to classroom studies, physiotherapy Bachelor’s programs typically include at least 1,000 hours of clinical rotations. After graduating, physiotherapists must register with regulatory boards in their countries/states and complete continuing education for licensure renewal.
Some physiotherapists opt to pursue Master’s degrees or Doctor of Physiotherapy (DPT) degrees as well, which can open up roles in teaching or research. So in some countries, education paths are converging with physical therapists.
Overall, physical therapists tend to have doctorate-level education, and physiotherapists more commonly have bachelor’s degrees. Both careers require rigorous coursework, clinical hours, and licensing exams to show competence. Continuing education keeps skills sharp in both professions.
Scope of Practice
Though their roles are extremely similar, there can also be slight variations in the scope of practice for physical therapists vs. physiotherapists:
Physical Therapist Practice
In most states, physical therapists can evaluate patients and develop treatment plans without physician referral. Services provided by PTs include:
- Performing exams and functional testing
- Diagnosing movement impairments
- Creating individualized treatment regimens
- Hands-on joint mobilization/manipulation
- Therapeutic exercise prescription
- Balance and gait retraining
- Designing/fitting assistive equipment like braces or artificial limbs
- Educating patients on prevention of re-injury
Some PTs choose specialty certifications to focus on areas like sports rehab, neurologic rehab, or pediatrics, for example. Overall, PTs play a major role in helping patients restore function after injury, surgery, or illness.
Physiotherapist Practice
Scope of practice for physiotherapists is extremely similar to that of PTs. Core services provided include:
- Patient assessments
- Manual therapy techniques
- Prescribing therapeutic exercises
- Administering electrotherapeutic modalities
- Fit patients with mobility aids like canes or wheelchairs
- Provide education on prevention of re-injury
In many countries, physiotherapists can evaluate and treat patients without physician referral as autonomous practitioners. Some key differences in a few areas though:
- In the US, PTs can order imaging or lab tests – physiotherapists typically cannot
- In some countries, physiotherapists have limited prescribing rights for medications. This does not apply to PTs in the US.
Like PTs, physiotherapists also pursue specialty certifications in preferred practice areas. But overall physiotherapists play the same critical role in helping patients regain strength, movement, balance, and coordination lost due to medical conditions, accidents, sports injuries, or surgeries.
Career Outlook and Salaries: Physical Therapist vs. Physiotherapist
The career demand for both physical therapists and physiotherapists is very strong. Here is an overview of salaries and job growth:
Physical Therapist Careers
The US Bureau of Labor Statistics predicts 21% job growth for physical therapists between 2020 and 2030, much faster than average. This amounts to an estimate of ~35,500 new PT job openings per year over the next decade.
The median pay for PTs in 2021 was $91,010 per year, or $43.74 per hour. Those with specialty certifications or working in hospitals or private outpatient centers tend to earn salaries on the higher end. The high job outlook and excellent pay make physical therapy an appealing, secure healthcare career choice.
Physiotherapist Careers
Similarly to PTs, the job outlook for physiotherapists is very strong across countries like Canada, the UK, Australia, and New Zealand. Many healthcare systems face physiotherapist shortages, so those entering the field have excellent job prospects.
Pay for physiotherapists is also quite good but varies more widely across different countries. Here’s a breakdown:
- USA: The average physiotherapist salary is $85,000 per year or $40.87 per hour
- Canada: The average salary for physiotherapists is $86356 CAD per year
- Australia – Median pay is $72,000 AUD annually
- United Kingdom – Average earnings are £32,800 per year
- New Zealand – Physiotherapists earn approximately $70,000 NZD on average
Now that we have covered the basic overview comparing physical therapists and physiotherapists, let’s drill down specifically into the physiotherapy profession.
In this extended section, we will explore various practice settings for physiotherapists, sub-specialties in the field, day-to-day roles, major professional organizations, and key considerations for those considering a career in physiotherapy.
Environments Where Physiotherapists Work
Physiotherapists can utilize their skills in a diverse range of settings serving varied patient populations. Some top work environments employing physiotherapists include:
Hospitals
Hospitals widely employ physiotherapists to help patients recovering from significant illnesses, accidents, surgeries, or medical events regain strength, mobility and independence with activities of daily living. Physiotherapists play especially crucial roles in injury rehabilitation and recovery on orthopedic, neurologic, or general medicine units.
In hospitals, physiotherapists conduct initial evaluations of patients, develop treatment plans, and provide interventions like therapeutic exercises, hands-on joint mobilization after surgery, training with mobility aids, educating patients on safe movements, scar tissue massage, and facilitating discharge planning.
Outpatient Clinics
Many physiotherapists work in private outpatient clinics and rehab centers serving patients who have undergone procedures like joint replacement, rotator cuff repair, or ACL reconstruction. Sports medicine clinics also employ many outpatient physiotherapists to serve athletes recovering from injuries.
In these settings, physiotherapists develop individualized exercise programs, utilize techniques like IASTM or cupping, give tailored home exercise regimens for self-care, and continually progress rehab. Appointments are longer to focus extensively on joint mobility, strength rebuilding, balance and agility.
Home Health Settings
Offering physiotherapy rehabilitation services directly in patients’ homes is also quite common. Home health allows treatment of clients who may have difficulties travelling outside the home for care – like elderly patients, pediatric patients, or those in postoperative recovery.
Physiotherapists make home visits to oversee therapeutic exercises, fit medical equipment like mobility aids, evaluate home layouts and activities to reduce fall risks, and ensure patients can safely perform daily life activities.
Aged Care Residences
In nursing homes, assisted living facilities, and aged care residences, physiotherapists serve integral roles in keeping elderly residents mobile and independent. As seniors experience functional decline after hospitalizations, fractures, strokes, or simply due to aging, intensive rehab helps maximize quality of living.
In these settings, physiotherapists focus on balance training to prevent falls, improving endurance for daily tasks, building muscle mass and strength through exercise, continually assessing equipment needs like wheelchairs or walkers, and teaching self-management strategies where possible.
Schools
Many school districts employ physiotherapists to serve students with disabilities, developmental delays like Down syndrome or Autism Spectrum Disorder (ASD), or recovering from significant injuries. School physiotherapists work with staff to integrate therapeutic activities into the classroom and shape customized support plans.
For children facing impairments impacting mobility skills or participation in age-appropriate activities, direct intervention by a pediatric physiotherapist can vastly improve positioning, coordination, peer interactions, and self-confidence.
Other Settings
Beyond hospitals, clinics, home health agencies, skilled nursing facilities, and schools, physiotherapists may also find job opportunities in a variety of other locations, like:
- Outpatient clinics associated with pro sports teams or athletic organizations
- Integrated health clinics and fitness centers
- Retirement communities, assisted living homes, and senior wellness centers
- Hospice organizations providing end-of-life care
- Workplace injury rehabilitation centers and employee health clinics
- Chronic pain management clinics
- Private individual and group practices
- Public health departments
- Research institutions and universities
- Defense system healthcare facilities

Physiotherapy Sub-Specialties
While some physiotherapists practice generalist roles across all types of patients, many choose to complete additional training and certifications to specialize in specific realms of therapy:
Orthopedic Physiotherapy
One of the largest branches of specialist practice is orthopedic physiotherapy, which focuses on muscular and skeletal issues like sports injuries, overuse syndromes, chronic arthritis, post-surgical rehabilitation, etc. Physiotherapists working in sports medicine or orthopedic outpatient clinics tend to sub-specialize in this domain.
Neurologic Physiotherapy
Many physiotherapists choose to specialize in treating patients with impairments stemming from traumatic spinal cord/brain injuries, strokes, multiple sclerosis, Parkinson’s disease, or other central nervous system disorders. Neurologic specialists help these patients regain function, balance, mobility, coordination, and independence in activities of daily living through targeted interventions.
Cardiopulmonary Physiotherapy
Some physiotherapists pursue additional education in treating patients with cardiac and/or pulmonary disorders like chronic obstructive pulmonary disease (COPD), cystic fibrosis, coronary artery disease, or those recovering from heart attacks, bypass surgery or heart/lung transplants. Cardiopulmonary physiotherapy utilizes breathing control exercises, activity tolerance regimens, and lung expansion techniques.
Geriatric Physiotherapy
With global populations aging, demand is very high for physiotherapists specifically trained in the needs of elderly patients. Geriatric specialists prescribe tailored exercise programs to improve strength, balance, mobility and reduce fall risks while also fitting adaptive equipment and teaching self-management strategies.
Pediatric Physiotherapy
Pediatric physiotherapists offer rehabilitation services tailored specifically to infants, children, and adolescents. These specialists address developmental delays, as well as recovery needs for conditions like torticollis, genetic disorders like Down syndrome, injuries, or post-surgical orthopedic needs in young patients.
Women’s Health Physiotherapy
Some physiotherapists complete additional training in women’s health realms like pre/postnatal care, pelvic pain management, treating urinary incontinence or other pelvic floor dysfunction. Services may include scar tissue massage after childbirth, pelvic floor muscle re-education, instruction of Kegel exercises, or diastasis recti recovery programs.
Additional Specialties
Beyond these common domains, physiotherapists can pursue all kinds of sub-niches depending on preferences, practice environments, particular patient demographics, and healthcare market demands. Further examples include:
- Vestibular Rehabilitation Therapy
- Hand Therapy
- Wound Care Therapy
- Lymphedema Management
- Oncology Rehabilitation
- Occupational Health/Ergonomics
- Pain Management
Building expertise as a specialist physiotherapist allows for delivery of highly customized and effective interventions tailored to each patient’s unique impairments, functional goals, lifestyle factors, and activity needs. Specialization also enables opportunities for private practice ownership.
Physiotherapist Roles
Now that we’ve covered various settings and specializations – what exactly does a physiotherapist do day-to-day? Core responsibilities include:
Patient Evaluations
A physiotherapist initially meets with new patients to conduct comprehensive evaluations discussing health history, onset of current symptoms, previous treatments, daily habits, medication usage, occupational demands, and more. They then perform objective physical assessments like range of motion testing, strength assessments, balance tests, or gait evaluations relevant to each patient’s situation.
Develop Treatment Plans
Based on assessment findings, physiotherapists develop highly-customized short and long-term treatment plans outlining therapeutic interventions aimed at returning patients to desired levels of movement and decreasing dysfunction or disabilities.
Administer Interventions
Physiotherapists offer a wide spectrum of hands-on interventions during patient appointments to address identified impairments. Techniques may include joint mobilization and manipulation, soft tissue massage, therapeutic cupping or needling, electrical stimulation modalities, prescription of assistive devices, and supervised therapeutic exercises.
Progress Reassessments
Physiotherapists continually re-evaluate patients throughout treatment courses to track progress towards established goals, adjust interventions accordingly, and document outcomes.
Patient Education
Physiotherapists provide extensive instruction to patients on topics like safe movement patterns, self-massage, proper use of ambulatory aids or orthotic devices, home exercise programs for maintenance, strategies for injury prevention, and more to encourage independence.
Coordinate Care
Physiotherapists communicate with physicians and other healthcare team members regarding patient progress and treatment recommendations. They help coordinate appropriate follow-up medical care or additional health services that may benefit clients.
Manage Staff
Physiotherapists may also oversee physiotherapy assistants, exercise physiologists, students, administrative staff, and other clinic personnel depending on their practice setting and seniority.
So in summary, physiotherapists wear many hats as evaluators, care planners, hands-on intervention providers, communicators, educators, and team managers collaborating to help clients regain optimal movement capability and physical function after setbacks.

Influential Physiotherapy Organizations
There are a number of influential membership organizations that support the growth of research, education, and evidence-based practice in physiotherapy:
World Physiotherapy
Formerly called WCPT until a 2021 name change, World Physiotherapy now represents the unified global voice advancing the entire physiotherapy profession. With a mission to support physiotherapist development, education, practice, and research around the world, World Physiotherapy contains 116 member organizations from countries across the globe.
Key activities of World Physiotherapy include building educational/credentialing frameworks, providing evidence-based clinical practice guidelines, facilitating international partnership opportunities and knowledge exchange, advocating for recognition of physiotherapy’s vital role within evolving healthcare systems, and giving physiotherapists representation in global policy discussions.
National Member Organizations
Individual countries have national physiotherapy associations that link back to World Physiotherapy similar to state chapters affiliating with a national entity. These member groups often advocate for the profession within their country, offer practice resources, facilitate research, provide leadership opportunities, host conferences and networking events, supply job boards, and publish journals or newsletters for the physiotherapy community.
Some examples include the Canadian Physiotherapy Association, Australian Physiotherapy Association, Chartered Society of Physiotherapy in the UK, Singapore Physiotherapy Association, South African Society of Physiotherapy, etc. Most countries with thriving physiotherapy professions have leading groups supporting growth.
Specialist Academies and Networks
In addition to national associations representing the physiotherapy profession as a whole, there are also subgroups focused around various specialty areas like sports physiotherapy, neurologic rehab, cardiopulmonary care, gerontology, pediatrics, pelvic health, orthopedics, and more.
These specialist member academies allow physiotherapists practicing in specific niches to collaborate on emerging research, clinical challenges, optimized interventions, new technologies, and further development of specialized skillsets within their realm of focus through shared conferences, journals, training materials and courses.
Academic Institutions
Top universities delivering physiotherapy training/education also have alumni societies and faculty-run organizations physiotherapists can join for networking and research circulation. Academic groups help new grads stay connected for mentorship opportunities, clinical visits, access to library resources, seminars, job postings, and more.
Membership in well-respected physiotherapy bodies, especially those with specialization focuses matching a practitioner’s niche interests and practice setting, offers excellent leadership guidance,skill development opportunities, career growth prospects, and peer community platforms.
Now that we’ve covered the basic comparison of physical therapists vs. physiotherapists, let’s drill down specifically into details of the physical therapy profession itself.
In this extended section, we’ll explore practice settings for physical therapists, sub-specialties in the field, day-to-day roles, major PT organizations, and considerations for those considering a career in physical therapy.
Environments Where Physical Therapists Work
Physical therapists have ample opportunities to utilize their clinical skills in diverse settings serving varied patient demographics. Some top work environments employing PTs include:
Hospitals
Hospitals widely employ physical therapists to serve patients recovering after significant medical events like illness, injury, or surgery. PTs play crucial roles in helping patients rebuild mobility, strength, and independence on specialty units like orthopedics, neurology, ICU, NICU, burn units, cardiopulmonary rehab, and general medicine floors.
In hospitals, PTs conduct initial evaluations, develop treatment interventions, provide hands-on therapies, train patients on adaptive equipment usage, educate on safe movement, recommend discharge arrangements, and help coordinate follow-up care.
Outpatient Clinics
Many physical therapists work in private outpatient clinics and dedicated rehab centers serving patients recovering from procedures like joint replacement, rotator cuff repair, spine surgery, or sports injuries. Athletics-focused PT clinics also serve athletes recovering from injuries or strains.
In these settings, PTs develop customized exercise programs, utilize techniques like IASTM or dry needling, prescribe home exercise modifications, continually progress rehab protocols, work to prevent re-injury through movement pattern corrections and strength rebuilding.
Home Health Settings
Delivering physical therapy care directly in patients’ homes following hospitalization can help serve individuals facing mobility limitations or unable to easily leave home – like elderly patients, pediatric patients, or those recovering postoperatively.
PTs make home visits to ensure appropriate home layouts/equipment, oversee therapeutic exercises, assess fall risks, fit medical devices like canes/walkers, and enable clients to safely perform daily life activities.
Skilled Nursing Facilities
In nursing homes, assisted living centers, and elder care residences – physical therapists provide integral rehabilitation services catered to aging adults and geriatric patients. As seniors experience functional decline after hospital stays, fractures, strokes, and general aging, intensive PT helps maximize mobility.
PTs in these settings focus on balance and gait training, building muscle strength via exercise, assessing equipment needs like wheelchairs, improving endurance for activities of daily living, prescribing maintenance programs, and teaching self-management strategies.
Schools and Early Intervention Programs
Many school districts employ physical therapists to serve children and adolescents with disabilities, developmental delays, congenital conditions like cerebral palsy or muscular dystrophy, or recovering from significant injuries. PTs work closely with education staff to integrate therapeutic strategies into classroom and recreation environments.
For infants and toddlers, PTs play a key role in early intervention programs – addressing impairments through positioning, strengthening, improving coordination, and encouraging age-appropriate motion to prevent contracture formation.
Other Settings
Aside from main locations like hospitals, clinics, patients’ homes, and schools – PTs may find abundant other opportunities, such as:
- Integrated Health Clinics
- Fitness and Wellness Centers
- Extended Care Retirement Communities
- Hospice and Palliative Care Organizations
- Employee Health and Workplace Injury Rehab Centers
- Chronic Pain Management Programs
- Defense and Veterans Health Systems
- Public Health Departments
- Clinical Research Centers
- Universities and Teaching Hospitals
- Private Individual/Group Practices
In summary – PTs can pursue careers in very diverse clinical settings spanning healthcare systems to community centers serving populations ranging from pediatric to geriatric.

Physical Therapy Specialties
While some PTs deliver generalized services to wide-ranging patient groups, many pursue board certifications and specialty training in specific realms like:
Orthopedic Physical Therapy
One of the largest specialty areas is orthopedic PT, which focuses on musculoskeletal conditions like sports injuries, chronic arthritis, overuse strains, postoperative rehabilitation, amputee limb fitting, and spinal conditions. Those PTs working in sports medicine clinics, orthopedic offices, or musculoskeletal programs focus on this realm.
Neurologic Physical Therapy
Many PTs choose to specialize in treating patients with impairments stemming from conditions impacting central nervous system function – like spinal cord injuries, traumatic brain injuries, strokes, Parkinson’s disease, multiple sclerosis, and muscular dystrophy. Neurologic PTs tailor interventions to improve patient mobility, balance, coordination, strength, and control.
Cardiopulmonary Physical Therapy
Some PTs complete intensive education in treating patients with cardiac and pulmonary disease processes, including post-heart attack recovery, coronary bypass rehabilitation, or breathing disorders like COPD, cystic fibrosis, and asthma. Cardiopulmonary PTs leverage breathing control techniques, activity tolerance progression, and chest mobility exercises.
Geriatric Physical Therapy
Specializing in care for older adults, geriatric PTs prescribe tailored treatment plans promoting mobility, strength, and physical independence within assisted living environments. These specialists also focus on fall prevention measures, fitness regimens for seniors, and prescribing adaptive equipment for aging patients.
Pediatric Physical Therapy
Pediatric PTs offer customized rehab services for infants, children, and adolescents – addressing impairments like torticollis, genetic conditions, injuries, developmental delays, and recovery after orthopedic surgery in young patients. Areas of focus include strength, motion, coordination, and encouraging participation.
Additional Specializations
Beyond top specialties noted above, PTs can pursue all kinds of sub-niches depending on interests, practice locations, patient demographics, and specific health needs. Some examples include:
- Women’s Health and Pelvic Floor Dysfunction PTs
- Wound Care Specialists
- Hand Therapy Experts
- Vestibular Rehabilitation Therapists
- Lymphedema Therapists
- Industrial and Ergonomic PTs
- Oncology Rehab Specialists
Specialist PTs deliver highly-customized interventions tailored to each patient’s unique functional goals, lifestyle factors, impairments and activity needs. Specialization also enables private practice opportunities serving niche patient groups.
Physical Therapist Roles
Now that we have outlined various settings and areas of sub-specialization – what are the day-to-day responsibilities involved in practicing as a PT? Core roles include:
Patient Evaluations
PTs initially collaborate with patients to gather health histories, discuss current symptoms, mobility challenges, pain levels, medications, daily activities, previous treatments, and impacts on occupational or life roles. PTs then perform in-depth objective physical evaluations like range of motion and strength tests, balance assessments, gait analysis, or functional movement screenings.
Develop Treatment Plans
Leveraging evaluation findings, PTs outline both short and long-term rehabilitation plans specifying progressive interventions aimed at enabling patients to return to the highest possible levels of functional independence and physical capability.
Deliver Interventions
PTs offer a spectrum of hands-on treatments during patient appointments to address identified mobility limitations, strength deficits, balance dysfunctions, coordination impairments, or activity restrictions. Techniques can include joint mobilization, therapeutic exercises, electrical stimulation modalities, manual therapy, adaptive equipment prescription and training.
Conduct Progress Reassessments
PTs continually re-evaluate patients throughout treatment to track gains towards established goals, gauge efficacy of current interventions, adjust therapy plans accordingly, and document functional outcomes.
Patient Education
PTs instruct patients on safe movement patterns, home exercise program compliance, proper use of mobility aids/braces, reinjury prevention protocols, postural awareness, joint protection techniques, self-massage, and developing long-term health and wellness habits.
Coordinate Care
PTs communicate with referring physicians, insurance case managers, other rehabilitation professionals, specialist healthcare providers, and community resources to coordinate seamless care continuation, follow-up medical services, access to support programs or networks, and appropriate ongoing care referrals when needed.
So in summary, PTs have diverse responsibilities spanning patient evaluations, hands-on service delivery, treatment planning, holistic care coordination, client education, and therapeutic progress tracking to enable patients to regain maximal physical strength, mobility, balance, and functional abilities.
Influential Physical Therapy Associations
There are numerous professional membership bodies supporting growth of research, best practice standards, continuing education, networking, policy advocacy, and career development for physical therapists:
American Physical Therapy Association (APTA)
The APTA represents over 100,000 PTs, PT assistants, and students within the United States as the leading membership organization advancing the physical therapy profession via advocacy campaigns, practice resource toolkits, evidence-based research, career development platforms, specialty section subgroups, grants, and more. The APTA hosts annual conferences for networking and learning opportunities to support PTs throughout their careers.
World Physiotherapy’s Physical Therapy International Network
World Physiotherapy contains a dedicated Physical Therapy International Network for connecting physical therapists globally. This global subgroup helps develop educational standards, clinical practice guidelines, advanced specialty training programs, and international research collaborations to advance the PT profession.
National Physical Therapy Associations
Many countries have national associations designed specifically to support the growth of physical therapy practice locally through advocacy, research funding, establishing codes of conduct, producing career resources and job boards, developing clinical practice guidelines for standardization, and elevating recognition of physical therapy’s value.
Some examples include the Canadian Physiotherapy Association, Chinese Physical Therapy Association, Korean Physical Therapy Association, Japanese Physical Therapy Association, etc. Countries with strong physical therapy workforces typically have leading professional associations.
Specialist Physical Therapy Academies
Reflecting the vast array of physical therapy specializations noted previously, there are professional academies and member networks focused explicitly around niche areas of practice like orthopedics, neurology, cardiopulmonary, geriatrics, pediatrics, and more.
These specialist groups facilitate collaboration among PTs focused on the same condition categories. Goals include advancing evidence-based interventions, optimizing treatment outcomes, elevating recognition of their specialty’s importance, launching targeted research projects, and hosting topic-specific annual conferences to support continuing niche education.
Academic Institutions
Finally, top colleges delivering physical therapy training and education also frequently have alumni networks and faculty-run organizations PTs can join post-graduation for continued access to mentorship opportunities, research circulation, library access, clinical visit invitations, seminars, job postings and more. Ongoing affiliation with academic institutions fosters career growth.
Main Points from The Comparison
Physical therapists:
- Typically complete Doctor of Physical Therapy (DPT) degrees in the United States
- Must pass national exam and fulfill state license requirements to practice
- Can evaluate and treat patients without physician referral in most states
- Scope encompasses therapeutic exercise, hands-on joint and soft tissue mobilization, modalities, equipment prescription, and patient education
- Practice in settings like hospitals, outpatient clinics, home health, skilled nursing facilities, schools, etc.
- Can pursue board certifications in specialties like orthopedics, neurology, cardiopulmonary, geriatrics etc.
- Influential organizations include the American Physical Therapy Association and World Physiotherapy International PT Network
- Very high job growth projected amid aging population and rise of chronic conditions
Physiotherapists:
- Most commonly complete bachelor’s degree programs in Physiotherapy
- Must register with regulatory boards to demonstrate qualifications to practice
- Scope is similar to physical therapists but with subtle variability in medical ordering abilities by region
- Practice in diverse settings like hospitals, home care, outpatient clinics, community centers, schools
- Can pursue specialized certifications in realms like orthopedics, neurology, geriatrics, cardiopulmonary, and more
- World Physiotherapy and national organizations provide support for career growth
- Continues to be high job demand and good salary prospects projected globally





